Electronic Brachytherapy (eBrachy or EB) is an advanced radiotherapy technique that delivers high-dose-rate (HDR) radiation using a miniaturized X-ray source, rather than traditional radioactive isotopes. Developed in the early 2000s as an alternative to conventional brachytherapy, EB emerged from innovations in miniaturized X-ray tube technology, with the first commercial systems like the Xoft Axxent introduced around 2006.
This method focuses radiation precisely on the target tissue while minimizing exposure to surrounding healthy areas, making it particularly suitable for superficial treatments. By 2025, EB has gained traction in oncology, especially for nonmelanoma skin cancers (NMSC), breast cancer (intraoperative radiation therapy or IORT), and other localized tumors, with ongoing clinical trials exploring broader applications. The global market for brachytherapy devices, including electronic variants, is valued at around USD 1-1.5 billion, with EB contributing a growing share due to its safety and convenience advantages. Leading systems include the Xoft Axxent (iCAD Inc.) and Esteya (Elekta), which have received FDA clearance and CE marking for various indications.

System Description and Technical Properties
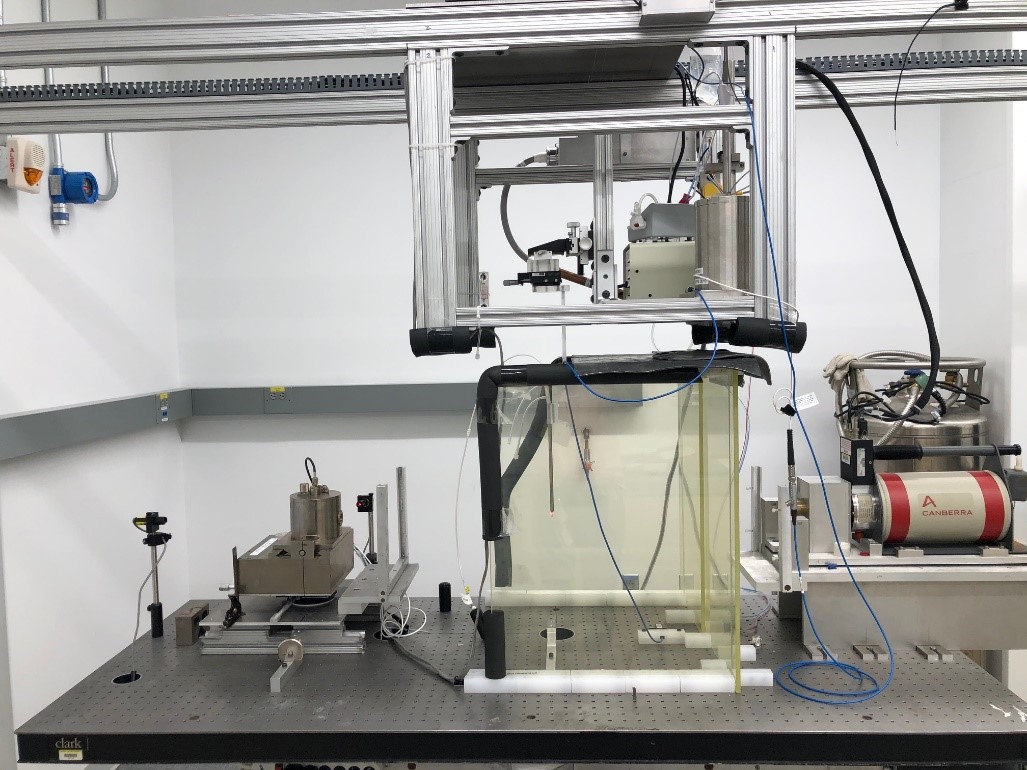
Electronic brachytherapy systems consist of a portable X-ray generator, typically operating at 50-100 kV, connected to applicators that deliver radiation directly to the treatment site. The core is a miniature X-ray tube (e.g., 2-3 mm diameter) that produces low-energy photons, allowing for steep dose fall-off and reduced penetration beyond the target. Key properties include:
Radiation Energy: 50-100 kVp, producing soft X-rays with effective half-value layers of 0.5-1.5 mm aluminum.
Dose Rate: High-dose-rate (HDR) delivery, typically 5-10 Gy/min, enabling short treatment times (3-10 minutes per session).
Applicators: Surface cones (for skin), balloon catheters (for breast), or custom shields; diameters range from 1-5 cm for precise targeting.
Portability: Systems weigh 10-30 kg, allowing use in outpatient settings without heavy shielding.
Radiation Output: Electronically controlled for precise dosimetry, with no radioactive decay or afterloading required.
The X-ray source is tungsten or gold-target based, with water or air cooling to manage heat during operation.
Production Methods
Electronic Brachytherapy Systems are manufactured using precision engineering for the X-ray tube and electronics. The process involves:
- X-ray Tube Assembly: Miniaturized tubes are fabricated with vacuum-sealed anodes (tungsten) and cathodes, using brazing or welding for hermetic seals.
-
Electronics Integration: High-voltage generators (up to 100 kV) and control systems are assembled with radiation shielding (lead or tungsten alloys)
-
Applicator Design: Custom molds for cones or catheters, often from medical-grade plastics or metals, with integrated dosimetry sensors.
-
Quality Control: Systems undergo calibration, leakage testing, and dosimetry verification to ensure uniform radiation fields and compliance with standards like IEC 60601.
Production is conducted in cleanroom facilities to meet medical device regulations, with materials like beryllium for X-ray windows to optimize transmission.
Applications and Uses
Electronic brachytherapy is primarily used for localized cancers where precise, superficial radiation is needed. Key applications include:
Nonmelanoma Skin Cancer (NMSC): Basal/squamous cell carcinomas; fractionated treatments (6-8 sessions) deliver 40-50 Gy with high cure rates (>95%) and good cosmesis.
Breast Cancer: Intraoperative partial breast irradiation (IORT) post-lumpectomy; single-dose (20-21 Gy) reduces treatment time from weeks to minutes.
Other Indications: Gynecological cancers (vaginal/cervical), keloids, and emerging uses in prostate or rectal tumors.
Advantages over isotope-based brachytherapy include no radiation safety concerns for storage/transport, on-demand activation, and customizable dose distributions.
Health and Safety Considerations
EB offers a safer profile than isotope brachytherapy, with no risk of radioactive contamination or long-term exposure. Radiation is only produced when powered on, reducing staff dose to near-background levels with proper shielding. Patient side effects are similar to other radiotherapies: Skin erythema, dryness, or ulceration in NMSC treatments, resolving within weeks; low rates of severe toxicity (<5%). Long-term risks include secondary malignancies, though lower due to shallow penetration. Contraindications include pregnancy, deep tumors, or pacemaker interference.
Environmental Impact
EB has a minimal environmental footprint, as it eliminates the need for radioactive waste disposal associated with isotope sources. Energy consumption is low during treatments, and systems are designed for longevity (tube life >1,000 hours). However, manufacturing involves metals like beryllium, requiring proper recycling to avoid toxicity.
Regulations and Recommendations
In the U.S., EB systems are FDA-cleared as Class II devices, requiring 510(k) premarket notification and adherence to radiation safety standards (21 CFR Part 1020). In Europe, CE marking under the Medical Device Regulation (MDR) ensures safety, with dosimetry calibrated to standards like IAEA TRS-398. Professional societies like ASTRO provide guidelines on patient selection and quality assurance. Recommendations include independent dosimetry verification, staff training, and ongoing clinical trials to expand indications. Future directions involve integration with imaging for adaptive therapy and expansion to deeper tissues via higher-energy sources.
More articles by ZMR Researche:
https://www.zionmarketresearch.com/de/report/gi-stool-testing-market
https://www.zionmarketresearch.com/de/report/quadricycle-and-tricycle-market
https://www.zionmarketresearch.com/de/report/ascites-market
https://www.zionmarketresearch.com/de/report/tendon-repair-market
https://www.zionmarketresearch.com/de/report/colon-cancer-diagnostic-market