Breast Cancer Detection refers to the processes and technologies used to identify breast cancer at its earliest possible stage, significantly improving prognosis and treatment success. Breast cancer is the most common cancer among women globally, with approximately 2.3 million new cases diagnosed annually as of recent estimates. It is the second leading cause of cancer death in women, though mortality rates have declined steadily due to advancements in early detection and treatment. Early-stage detection (localized disease) yields five-year survival rates exceeding 99%, compared to around 30% for metastatic cases.
Detection strategies encompass self-awareness, clinical examinations, imaging modalities, and confirmatory diagnostics. Guidelines from organizations like the American Cancer Society (ACS), U.S. Preventive Services Task Force (USPSTF), and World Health Organization (WHO) emphasize risk-based screening to balance benefits against potential harms like overdiagnosis and false positives.
Risk Factors and Prevention
Effective detection begins with understanding risk. Major non-modifiable risks include:
- Age (risk rises sharply after 50).
- Genetic mutations (BRCA1/BRCA2 account for 5-10% of cases).
- Family history.
- Dense breast tissue (reduces mammography sensitivity).
- Prior radiation exposure or certain benign breast conditions.
Modifiable risks involve lifestyle: obesity (post-menopause), excessive alcohol, physical inactivity, hormone replacement therapy, and delayed or no childbearing. Preventive measures include maintaining healthy weight, limiting alcohol, regular exercise, and for high-risk individuals, chemoprevention (e.g., tamoxifen) or prophylactic surgery.
Genetic counseling and testing are recommended for those with strong family history, guiding intensified surveillance.
Breast Self-Examination (BSE)
BSE is a low-cost, accessible method empowering individuals to monitor changes. Performed monthly (post-menstruation for premenopausal women), it involves:
- Visual inspection for asymmetry, dimpling, or nipple changes.
- Palpation in circular, vertical, or wedge patterns while lying and standing/showering.
While BSE alone does not reduce mortality in population studies, it promotes awareness and prompts timely medical consultation when abnormalities (lumps, thickening, discharge) are found.
Clinical Breast Examination (CBE)
Performed by healthcare professionals during routine visits, CBE complements BSE. It detects palpable masses or abnormalities missed by patients. Sensitivity varies (40-70%), but it remains valuable in low-resource settings or as an adjunct to imaging.
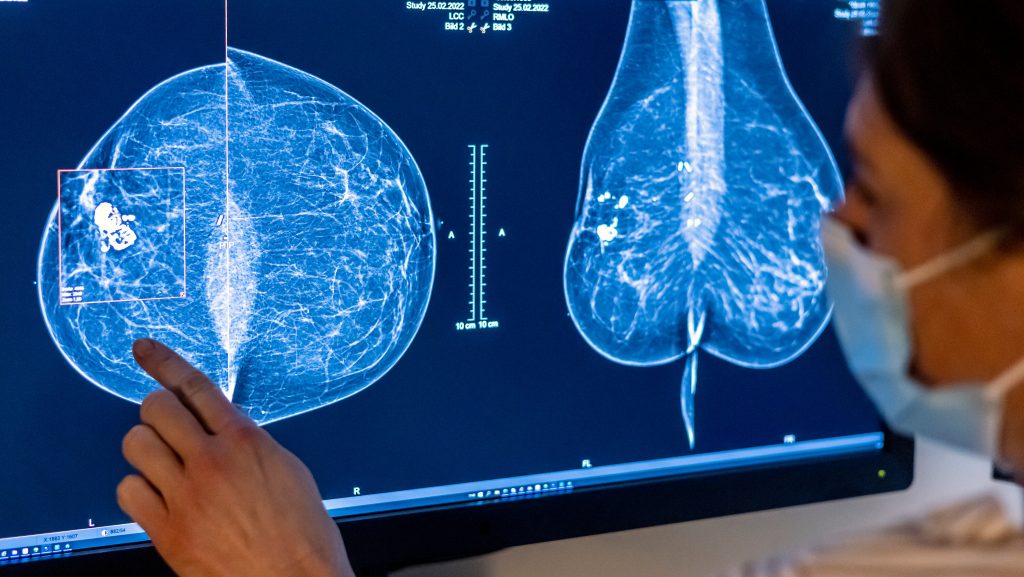
Mammography
Digital mammography is the cornerstone of population-based screening. It uses low-dose X-rays to produce breast images, detecting microcalcifications or masses years before palpability.
- Screening Guidelines: ACS recommends annual mammograms starting at age 45 (optional 40-44); USPSTF biennial from 50-74. High-risk women start earlier/more frequently.
- Types: 2D digital; 3D tomosynthesis (DBT) reduces recall rates by 15-20% and improves cancer detection by 20-40%, especially in dense breasts.
- Performance: Sensitivity 85-90% overall; lower (~60%) in dense breasts. Specificity ~90%, leading to false positives requiring follow-up.
Benefits: 20-40% mortality reduction in screened populations. Harms: Radiation exposure (minimal), anxiety from recalls, overdiagnosis of indolent cancers.
Ultrasound
Breast ultrasound uses sound waves for real-time imaging, excelling at distinguishing solid masses from cysts. It serves as:
- Adjunct to mammography for dense breasts (supplemental screening detects additional 2-4 cancers per 1,000).
- Diagnostic tool for palpable abnormalities or mammographic findings.
Automated whole-breast ultrasound (AWBUS) standardizes scans, improving reproducibility. Handheld ultrasound is operator-dependent but widely available.
Magnetic Resonance Imaging (MRI)
Contrast-enhanced breast MRI offers highest sensitivity (>90%) for invasive cancers. Indications:
- Screening high-risk women (annual with mammography).
- Evaluating extent in known cancer.
- Problem-solving ambiguous findings.
Abbreviated protocols shorten scans to 10-15 minutes, enhancing accessibility. Limitations: High cost, false positives, gadolinium contrast risks.
Other Imaging Modalities
- Molecular Breast Imaging (MBI)/Breast-Specific Gamma Imaging: Uses radiotracers; useful in dense breasts (sensitivity ~90%).
- Contrast-Enhanced Mammography (CEM): Combines mammography with iodinated contrast; comparable to MRI for some indications.
- Thermography: Measures infrared heat; lacks evidence for screening (not recommended by major guidelines).
Biopsy and Pathology
Suspicious findings require tissue sampling for definitive diagnosis:
- Fine-Needle Aspiration (FNA): Quick cytology.
- Core Needle Biopsy (CNB): Preferred; provides histology (image-guided: ultrasound, stereotactic, MRI).
- Vacuum-Assisted/Surgical Biopsy: For larger samples or calcifications.
Pathology assesses tumor type (ductal/lobular), grade, hormone receptors (ER/PR), HER2 status, guiding therapy.
Emerging and Future Technologies
- Artificial Intelligence (AI): Algorithms analyze mammograms, reducing false negatives/positives and radiologist workload. Systems achieve 90%+ accuracy, with some outperforming humans in dense breasts.
- Liquid Biopsy: Circulating tumor DNA (ctDNA) detection for minimal residual disease or screening (research stage).
- Risk-Based Screening: Polygenic risk scores + density for personalized intervals.
- Optical Imaging/Photoacoustics: Non-ionizing alternatives under investigation.
Challenges and Considerations
- Equity: Access disparities in low-resource areas.
- Overdiagnosis: 10-20% of screen-detected cancers may not progress.
- Radiation: Cumulative exposure concerns.
- Dense Breasts: Supplemental screening debates.
Guidelines evolve with evidence; shared decision-making is key.
Conclusion
Breast cancer detection has advanced dramatically, combining traditional imaging with emerging tools for earlier, more accurate identification. Regular screening per guidelines, awareness of personal risk, and prompt evaluation of symptoms remain cornerstone strategies for reducing burden and improving survival. Ongoing research promises further precision and accessibility.
More articles by ZMR Researche:
https://www.zionmarketresearch.com/de/report/wide-body-aircraft-mro-market
https://www.zionmarketresearch.com/de/report/freight-transport-market
https://www.zionmarketresearch.com/de/report/intraoperative-neuromonitoring-market
https://www.zionmarketresearch.com/de/report/fishing-rod-market
https://www.zionmarketresearch.com/de/report/car-t-cell-therapy-market