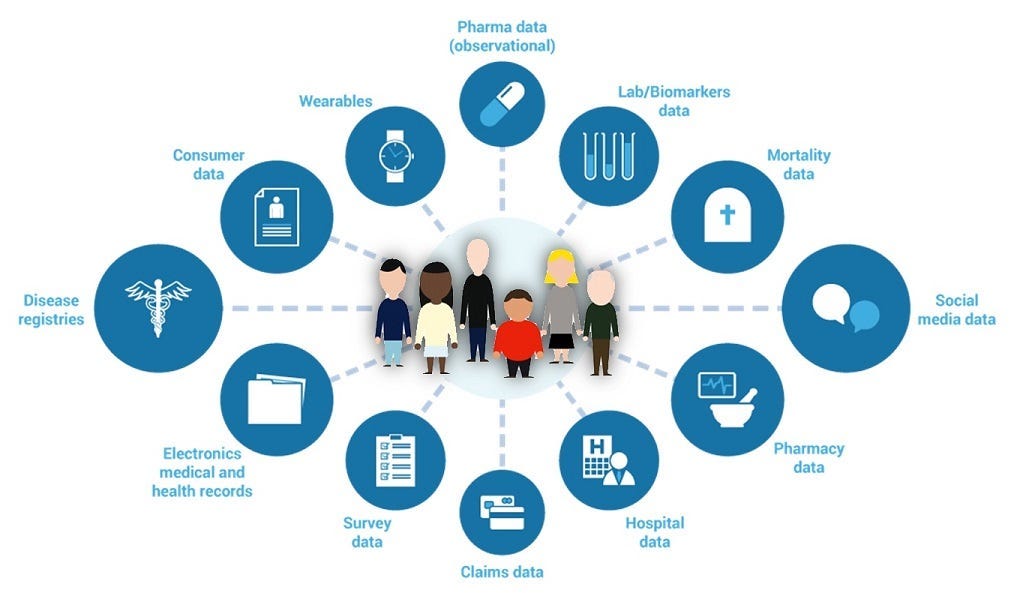
Psychiatric digital biomarkers are measurable physiological, behavioral, or cognitive indicators derived from digital data sources that can signal the presence, severity, progression, or treatment response of mental health conditions. These biomarkers are collected passively or actively through everyday devices such as smartphones, wearables, voice assistants, and social media platforms, leveraging sensors for metrics like voice patterns, movement, sleep, typing behavior, and facial expressions. Unlike traditional biomarkers (e.g., blood cortisol levels or brain scans), digital biomarkers offer continuous, real-time, non-invasive monitoring in natural environments, enabling early detection, personalized interventions, and objective assessment of psychiatric disorders.
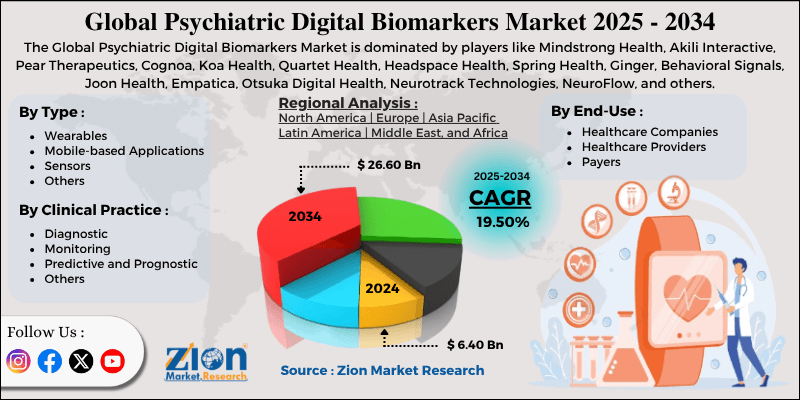
The concept emerged in the early 2010s with advances in mobile health (mHealth) and artificial intelligence (AI), building on earlier wearable tech for physical health. Pioneering studies, such as those from the University of Michigan and Harvard in the mid-2010s, demonstrated how smartphone data could predict mood swings in bipolar disorder or depressive episodes. By 2025, psychiatric digital biomarkers have transitioned from research tools to clinical applications, integrated into apps like Mindstrong (acquired by SonderMind) and BiAffect, and platforms from companies like Medtronic and Verily (Google’s health arm). The global market for digital biomarkers in mental health is valued at approximately USD 1.5-2 billion as of 2026, growing at 20-25% CAGR driven by rising mental health awareness post-COVID-19, AI advancements, and the push for remote monitoring amid healthcare shortages. Major players include Cognito Therapeutics, BlackThorn Therapeutics, and partnerships between tech giants (Apple, Google) and pharma (Pfizer, Novartis).
Psychiatric Digital Biomarkers represent a paradigm shift in mental healthcare, moving from subjective self-reports and episodic clinical visits to objective, continuous data streams that could revolutionize diagnosis, treatment, and prevention.
The Science Behind Psychiatric Digital Biomarkers
Psychiatric disorders like depression, anxiety, bipolar disorder, schizophrenia, and PTSD often manifest through subtle changes in behavior, cognition, and physiology. Traditional diagnostics rely on clinician interviews and questionnaires (e.g., PHQ-9 for depression), which are subjective, recall-biased, and infrequent. Digital biomarkers address this by capturing passive data from sensors and active inputs from apps, analyzed via machine learning (ML) algorithms to detect patterns correlated with symptoms.
Key Data Sources and Biomarkers
- Voice and Speech Analysis
- Metrics: Pitch variability, speech rate, pauses, tone.
- Applications: Slower speech and reduced prosody indicate depression; rapid/pressured speech signals mania in bipolar.
- Tech: AI apps like Ellipsis Health use smartphone microphones; studies show 80-90% accuracy in mood detection.
- Facial Expressions and Eye Tracking
- Metrics: Micro-expressions, gaze patterns, blink rate.
- Applications: Reduced facial mobility in depression; erratic gaze in ADHD.
- Tech: Webcam-based tools (Affectiva, now Smart Eye); integrated in telepsychiatry.
- Activity and Movement Tracking
- Metrics: Steps, acceleration, geolocation variability.
- Applications: Reduced mobility in depression; hyperactivity in mania/ADHD.
- Tech: Wearables (Fitbit, Apple Watch); accelerometer data predicts relapse in schizophrenia with ~75% accuracy.
- Sleep and Circadian Rhythms
- Metrics: Sleep duration, REM cycles, wake times.
- Applications: Disrupted sleep in anxiety/PTSD; irregular patterns in bipolar.
- Tech: Actigraphy from smartwatches; Oura Ring integrates with mental health apps.
- Digital Phenotyping from Smartphones
- Metrics: Typing speed, app usage, social media patterns, screen time.
- Applications: Slower keystrokes in depression; increased isolation (fewer calls/texts).
- Tech: Apps like Beiwe (Harvard) collect passive data; ML models detect symptoms early.
- Physiological Sensors
- Metrics: Heart rate variability (HRV), skin conductance, EEG from wearables.
- Applications: Low HRV in anxiety; stress responses in PTSD.
- Tech: Empatica E4 wristband; Muse EEG headband.
These biomarkers are processed using AI/ML algorithms (e.g., random forests, neural networks) trained on large datasets (e.g., BiAffect’s 20,000+ user database) to generate predictive scores or alerts.
Biological and Neurological Basis
Digital biomarkers correlate with neurobiological changes:
- Depression: Reduced dopamine/serotonin → lethargy, flat affect (detected in movement/speech).
- Anxiety: Hyperarousal → high HRV variability, rapid speech.
- Bipolar: Manic phases → increased activity/social interactions.
Integration with genomics (polygenic risk scores) and traditional biomarkers (cortisol) enhances accuracy.
Applications in Psychiatric Practice
Psychiatric digital biomarkers are transforming mental health care:
- Early Detection and Diagnosis
- Screening: Apps like Moodpath or SPARX use voice/activity data for initial assessments, flagging risks for professional follow-up.
- Differential Diagnosis: Distinguish depression from bipolar (e.g., activity patterns).
- Monitoring and Relapse Prevention
- Continuous Tracking: Wearables detect symptom escalation (e.g., decreased sleep signaling mania).
- Personalized Interventions: AI alerts prompt medication adjustments or therapy sessions.
- Treatment Response Evaluation
- Objective Metrics: Track improvements post-therapy or medication (e.g., increased activity after antidepressants).
- Research and Drug Development
- Clinical Trials: Biomarkers as endpoints (e.g., FDA-qualified for depression).
- Big Data: Large-scale studies (e.g., Apple Heart/Mind Study) aggregate anonymized data.
- Telepsychiatry Integration
- Remote Monitoring: Platforms like Ksana Health combine app data with virtual visits.
- Public Health and Population Screening
- Workplace Wellness: Corporate programs detect burnout.
- School Mental Health: Apps screen for adolescent anxiety/depression.
Adoption: >50% U.S. psychiatrists use some digital tools; Europe leads in integrated systems (e.g., NHS apps).
Benefits of Psychiatric Digital Biomarkers
- Objectivity: Reduces bias in self-reports.
- Continuous Data: Captures real-world fluctuations.
- Accessibility: Low-cost, scalable via smartphones (2.8 billion users worldwide).
- Early Intervention: Detects prodromal symptoms (e.g., subtle voice changes in schizophrenia relapse).
- Personalization: AI tailors treatments.
- Stigma Reduction: Private, non-clinical monitoring.
Studies: 2024 meta-analysis (JAMA Psychiatry) shows 70-85% accuracy in mood disorder detection.
Challenges and Limitations
Despite promise, barriers exist:
- Privacy and Ethics: Data security (HIPAA/GDPR); consent for passive collection.
- Accuracy and Validation: Variable across populations/devices; FDA-cleared apps rare.
- Digital Divide: Access for low-income/elderly.
- Over-Reliance: May miss nuanced symptoms.
- Algorithm Bias: Training data often Western-biased.
- Regulatory Gaps: Many apps unregulated as “wellness” tools.
2025 concerns: AI hallucinations in symptom interpretation.
Future Directions
By 2030:
- Multimodal Integration: Combine voice, activity, HRV with AI for 90%+ accuracy.
- Wearable Advancements: Smart earbuds (voice/EEG), rings (sleep/HRV).
- Theranostics: Biomarker-guided therapy (e.g., app-recommended CBT).
- Global Equity: Low-cost apps for LMICs.
- Ethical AI: Transparent algorithms, bias audits.
Research: NIH-funded projects on digital phenotyping for suicide prevention.
Conclusion
Psychiatric Digital Biomarkers revolutionize mental health by translating everyday digital signals into actionable insights for detection, monitoring, and personalized care. From voice analysis for depression to activity tracking for bipolar, they bridge gaps in traditional psychiatry, offering objective, continuous data. Benefits—early intervention, stigma reduction—are tempered by privacy and accuracy challenges. As AI matures and regulations evolve, these biomarkers promise more equitable, proactive mental healthcare. Informed use, ethical frameworks, and rigorous validation will maximize their transformative potential.
More articles by ZMR Researche:
https://www.zionmarketresearch.com/de/report/track-dumper-market
https://www.zionmarketresearch.com/de/report/vr-fitness-game-market
https://www.zionmarketresearch.com/de/report/vegetable-hpmc-capsule-market
https://www.zionmarketresearch.com/de/report/cell-line-development-market
https://www.zionmarketresearch.com/de/report/digital-gaussmeters-market