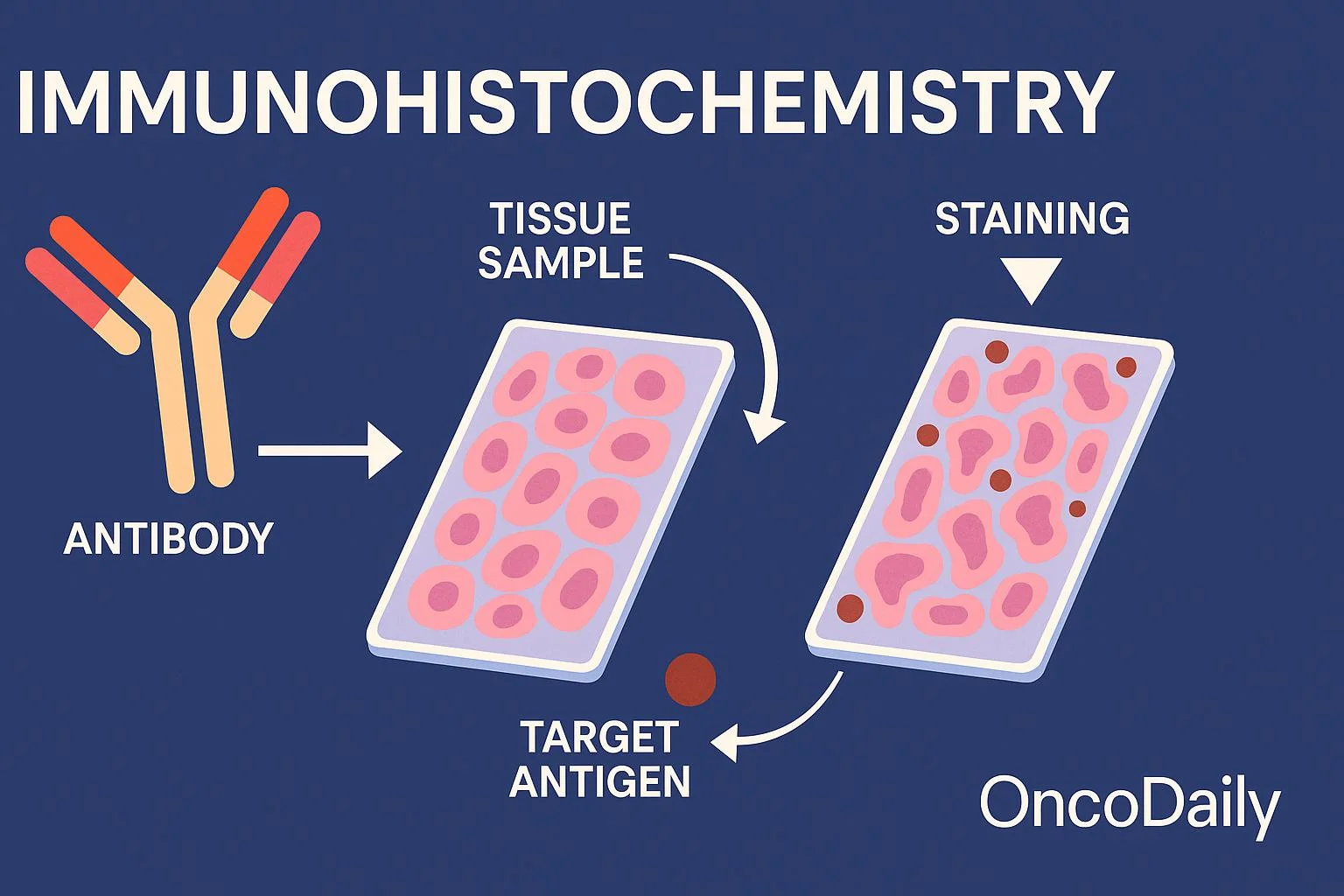
Immunohistochemistry (IHC) is a powerful laboratory technique used to visualize the presence, distribution, and localization of specific antigens (usually proteins) in tissue sections or cells through antigen-antibody interactions. By combining immunological and histological methods, IHC employs antibodies labeled with visible markers to detect targets, producing colored or fluorescent signals under a microscope.
Developed in the mid-20th century, IHC has become indispensable in pathology for diagnosing diseases, particularly cancers, infectious diseases, and autoimmune conditions. It enables pathologists to identify cell types, assess protein expression levels, and guide treatment decisions, such as in biomarker testing for targeted therapies.
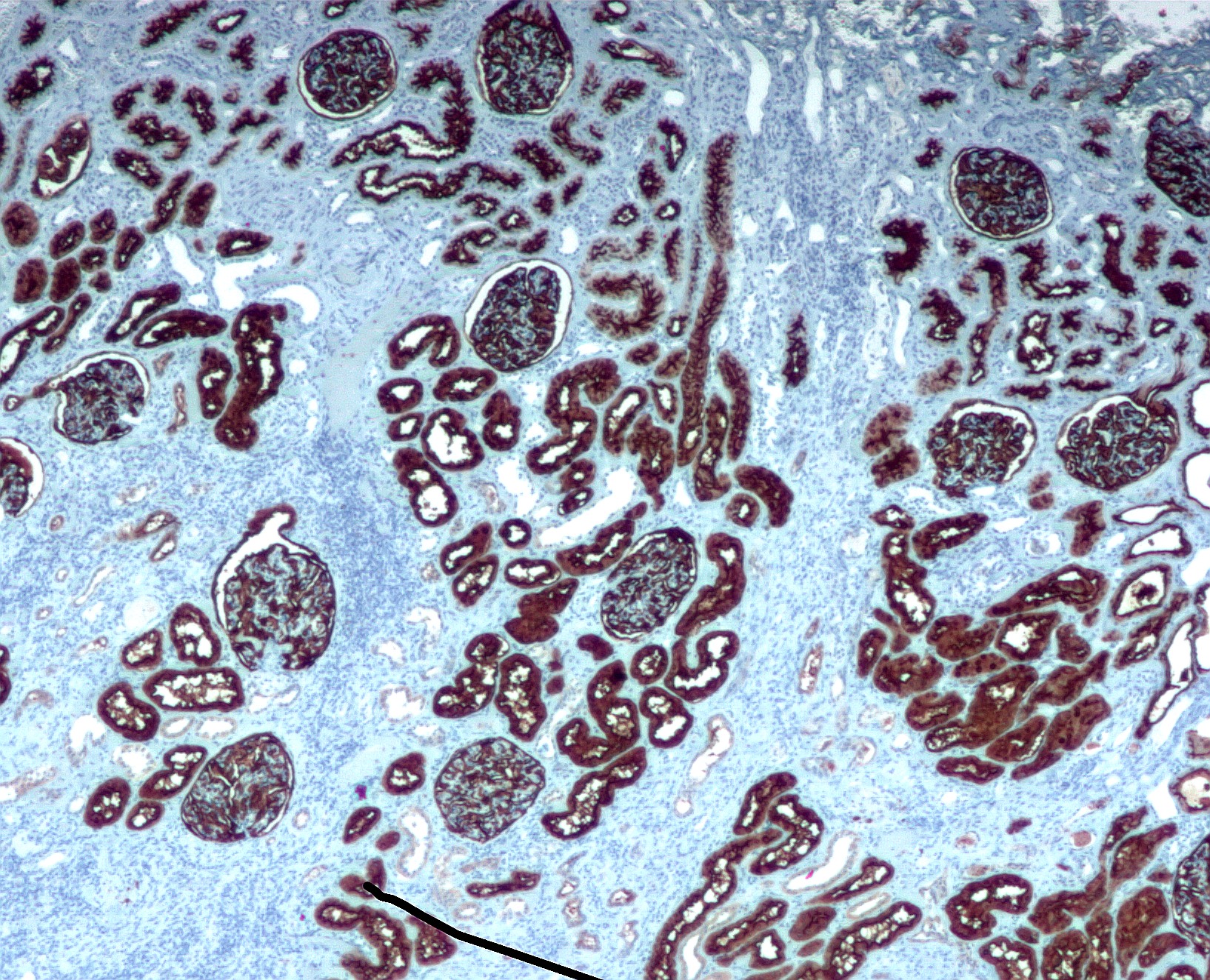
Classic example of IHC staining showing different patterns in tissue sections.
Brightfield IHC image of lung tissue highlighting specific protein expression.
Principles of Immunohistochemistry
IHC relies on the specific binding of antibodies to antigens. Primary antibodies recognize the target protein, while secondary antibodies (conjugated to enzymes or fluorophores) amplify the signal.
Key components:
- Antigens: Target molecules, often proteins.
- Antibodies: Monoclonal (highly specific) or polyclonal.
- Detection systems: Chromogenic (e.g., DAB producing brown color) or fluorescent.
- Controls: Positive/negative to validate results.
The technique exploits epitope-paratope specificity, with signal amplification to detect low-abundance targets.
Examples of true positive, true negative, and false positive IHC staining.
The IHC Protocol: Step-by-Step Process
A standard IHC workflow involves several critical steps to ensure accurate staining.
- Tissue Preparation and Fixation: Samples are fixed (usually in formalin) to preserve structure and antigens.
- Embedding and Sectioning: Paraffin embedding, then cutting thin sections (4-5 μm).
- Deparaffinization and Rehydration: Remove wax and rehydrate slides.
- Antigen Retrieval: Heat or enzymatic treatment to unmask epitopes hidden by fixation.
- Blocking: Prevent non-specific binding.
- Primary Antibody Incubation.
- Secondary Antibody and Detection.
- Counterstaining (e.g., hematoxylin for nuclei).
- Mounting and Visualization.
Detailed step-by-step diagram of the IHC process.
Another illustrative workflow for IHC staining.
Signal amplification methods commonly used in IHC.
Types of IHC
Chromogenic IHC
The most common, using enzymes like horseradish peroxidase (HRP) with substrates like DAB for permanent brown staining. Ideal for routine diagnostics.
Typical chromogenic IHC on spleen tissue showing dual staining.
Fluorescent IHC (Immunofluorescence)
Uses fluorophores for multi-color labeling, viewed under fluorescence microscopy.
Multiplex fluorescent IHC allowing simultaneous detection of multiple markers.
Another example of multiplex immunofluorescence focusing on immune cell clusters.
Multiplex IHC
Advanced techniques (e.g., tyramide signal amplification or mass spectrometry-based) enable detection of 10+ markers on one slide, crucial for tumor microenvironment analysis.
Applications of IHC
- Cancer Diagnosis and Prognosis: Markers like HER2, ER/PR in breast cancer; PD-L1 for immunotherapy eligibility.
- Infectious Diseases: Detecting pathogens (e.g., viral antigens).
- Research: Protein localization, pathway analysis.
- Neuropathology: Amyloid plaques in Alzheimer’s.
- Companion Diagnostics: Guiding personalized medicine.
High-magnification IHC stained slide under microscope.
Advantages and Limitations
Advantages:
- High specificity and sensitivity.
- Preserves tissue architecture.
- Widely available and cost-effective for chromogenic.
Limitations:
- Subjective interpretation.
- Antigen masking from fixation.
- Cross-reactivity and background staining.
- Time-consuming manual process (though automation helps).
Positive and negative staining examples across different markers.
Automation and Modern Advances
Automated stainers (e.g., from Leica, Ventana, Dako) improve reproducibility and throughput in clinical labs.
Emerging trends include digital pathology, AI-assisted scoring, and spatial transcriptomics integration.
Conclusion
Immunohistochemistry remains a cornerstone of modern pathology and research, bridging immunology and histology to provide critical insights into disease mechanisms and patient care. Ongoing innovations in multiplexing, automation, and digital analysis continue to expand its capabilities, making IHC more precise and informative than ever.
More articles by ZMR Researche:
https://www.zionmarketresearch.com/de/report/events-industry-market
https://www.zionmarketresearch.com/de/report/liquid-crystalline-polymers-market
https://www.zionmarketresearch.com/de/report/medical-device-complaint-management-market
https://www.zionmarketresearch.com/de/report/bathroom-partitions-market
https://www.zionmarketresearch.com/de/report/5g-services-market





